Seniors are a select group of people that need extra care. Therefore, they usually have a line of products specifically made for them. One of these is the microwave. In case you are looking for the perfect microwave for a senior member of your family, The Ponfish’s Post would be a good starting point. In this article, we will look at some of the questions people frequently ask about senior microwaves. I hope that these will help you settle on the best. Senior microwaves faqs What makes a microwave suitable for seniors? You have to understand that not all microwaves suit seniors. Here are some of the distinct features that…
-
-
Best Cheap Gaming Laptops for Fallout 4 Under $500
Best Cheap Gaming Laptops for Fallout 4 Under $500
-
What is the best double jogger stroller for buy?
When we gave birth to our first child, Ellis, we bought Baby Jogger City Mini. He has been 19 months old and I cherish it very much. We live on the first floor in London, so I need a light carriage, which is difficult to carry everywhere. City Mini checked all containers. When I got the second smallest seat, 15 months later, it seemed easy to decide to get a dual format-one seat after another.
-
Is The Mintlyfe Patch Legit?
If you have visited Facebook recently, you may have seen an ad for Mintlyfe Patch. The abdomen-sized peppermint extract uses the conductivity of sophorosides and transdermal technology to promote weight loss and fat removal. Each patch contains a cocktail of 56 ingredients, including mint, Korean ginseng and capsaicin. These ingredients are regarded as the key to quickly and safely get rid of fat accumulation and cellulite in the "fluffy" area. A big promise was made, so I decided to test…
-
Breastfeeding and the Working Moms
Can I continue breastfeeding after I return to work?Yes, you can. If you live in a nearby workplace or at a daycare center on site or nearby, you can take a break from nursing time to feed your baby. If this is not possible, there are two options:
-
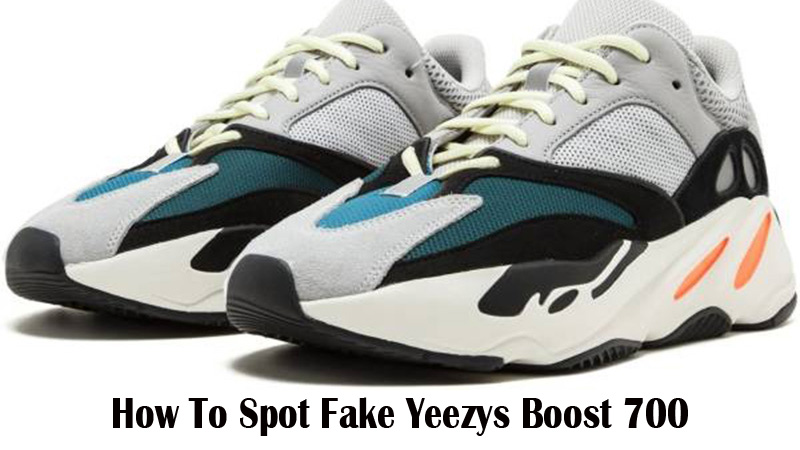
How To Spot Fake Yeezys Boost 700
Are you wondering how to discover the fastest method of Yeezy Boost 700 Wave Runner (OG)?If you don’t mind adding another pair of stylish Yeezy to the spin, you should choose Yeezy Boost 700 OG.
-
How to detect fake Adidas Yeezy Boost 750?
If you can't get a rating for the "Light Gray Yeezy Boost 750" launched on June 11, you may want to snap up a pair on eBay, Craigslist and other sites. Be sure to go out and buy things, but arm yourself as much as possible to avoid eventually getting counterfeit products.
-
Craft Fair Tips 2020
What's new in the artisan world? I am focused on helping you set up the craft exhibition. The appearance is beautiful but not crowded, and the attractive display determines whether the partons will stop or continue walking. I list some important elements and then discuss them in detail.
-
How to Safely Store Breast Milk?
If you are breastfeeding your baby and want to work again, you may need to start expressing milk and storing it for future use. Expression and storage can also make your routine more flexible. For the safety of infants, breast milk needs to be stored safely. Read tips on storing breast milk.
-
Working at home as a family carer: is it possible?
The cost of family care is sufficient without losing more income during the trip. Working from home is an option that can help you provide parental care while still providing financial services. Although not everyone can choose, working from home is becoming more common. Working at home as a family carer: is it possible?
-
Four Vaccines Urged for Seniors
I saw this article and thought it would be good information to pass on to you. We all thought we were done with vaccines once we reached adulthood. It’s important to check with your doctors to ensure you’re still up to date with important shots so you can proactively avoid some of the diseases that can be so detrimental to senior’s health. In the 1920s, the respiratory disease diphtheria was one of parents’ biggest fears for their children. In the United States, an estimated 100,000-200,000 cases of diphtheria per year caused 13,000-15,000 deaths, mainly children, in that decade (Wikipedia). Today, diphtheria vaccines have largely eradicated the disease from the United States.…
-
10 Holiday Gifts Seniors Want But Won’t Ask For
What do you get Grandma this year? A new blanket . . . again? How about a pair of slippers? While those gifts could satisfy the needs or desires of a senior loved one, why not choose a present that is even more meaningful: a gift from the heart. While you may not be able to add the following 10 gift ideas to a shopping list, you can bet they’re on your loved one’s wish list. Take your loved one shopping. Whether a trip to the mall or an online shopping spree, make it a special day. Be sure to tune into your loved one’s limitations and don’t overdo. Lend…
-
Seniors Face Challenges in Finding Work
I am a member of the Society of Certified Senior Advisors and receive a monthly newsletter that always has articles I think you’ll find interesting. This one is for Seniors who are looking for jobs. The article offers some really good tips and resources for even more information. If you’re interested in being a CAREGiver or know somebody who is, Home Instead Senior Care is always looking for people. Visit our website at www.makeadifferenceforseniors.com for more information. ——————————————————————————————————————————————————- Not only has the 2008 recession put a dent in a lot of retirement accounts but people are living longer, so it makes financial sense to keep working as long as you can,…
-
One Portland Family’s Experience with Home Instead Senior Care
I regularly have the thrill of reading notes of gratitude from clients or their family members. It’s so satisfying to hear about how much our CAREGivers meant to them or how much they appreciated the responsiveness, availability, and sensitivity of the office team. However, the letter I received last week from a client’s daughter just took the cake…had me smiling for days. I don’t like to brag, BUT, I really want to share this letter as a tribute to my wonderful CAREGivers and office staff who were there for this family in so many ways. For those of you who make it all the way through the letter, thanks for…
-
Adaptive Clothing for Seniors
As I work with seniors, families and caregivers, we eventually have issues concerning clothing. Sometimes the issue is due to arthritic fingers that can no longer button, hook, tie or zip. Sometimes it is impaired vision, and they are unable to put outfits together or see the fabric colors. Sometimes we have family members with dementia who take clothing off as soon as someone helps them get it on or who just need the simple closure styles. Frequently family members get frustrated because they do not know what to buy or where to shop. I have used the Buck and Buck Catalog for years to help families deal with these…
-
Baby Doll Therapy for Memory Care Residents
The Spectrum of Behaviors and Emotions Day by day we see residents that exhibit a complete spectrum of behaviors and/or emotions. Situations that arise in the early morning, will certainly give way for something new by the afternoon. This goes hand in hand with delivering quality dementia and Alzheimer’s care. Providing an environment that allows for these rapid, daily changes is a challenging and daunting task. As well as, learning how to provide “happiness” and “comfort” to a person with a declining mental state. Happiness Defined Happiness can be defined as simply as this, “the satisfaction of needs.” The needs, however, can change from age to age, year to year…
-
Quick Answer: How Long Do Goats Live
Goat/Lifespan. How long do goats live as pets? Goats live an average of 7-14 years, depending on breed. Diet, living conditions, and other factors also affect the lifespan of the
-
Question: How To Get Rid Of Chiggers
Washing with soap and water after outdoor activity may remove any chiggers that may be migrating on the skin and prevent their bites. Likewise, washing clothing that was worn outdoors
-
How Many Calories Are In An Egg
Egg/Energy Amount. How much calories is in 2 eggs? How Many Calories in Two Eggs? An average serving size of two eggs contains only 148 calories or 620 kilojoules –
-
How Cold Can Chickens Tolerate
What is this? Cold weather chickens can withstand temps around or slightly below freezing (32 degrees Fahrenheit to about ten degrees Fahrenheit). What temp is too cold for chickens? Chickens
-
Quick Answer: How To Get Rid Of Aphids
HOW TO GET RID OF APHIDS NATURALLY Remove aphids by hand by spraying water or knocking them into a bucket of soapy water. Control with natural or organic sprays like
-
How Long Do Ducks Live
Duck/Lifespan. How long do ducks live as a pet? They are relatively long-lived pets—it's possible for them to live 10-15 years when well cared for. Keep in mind that they
-
Question: When To Harvest Sunflower Seeds
Harvest when seeds are plump and developed. Harvest when flower petals begin to dry out and fall off. Harvest when the back of flower turns from green to yellow (if
-
What Caused The Dust Bowl
What circumstances conspired to cause the Dust Bowl? Economic depression coupled with extended drought, unusually high temperatures, poor agricultural practices and the resulting wind erosion all contributed to making the
-
Quick Answer: How To Get Rid Of Yellow Jackets
What is a home remedy to get rid of yellow jackets? Mix 1 tablespoon of detergent and 2 cups of water. Alternatively, mix equal parts of water and liquid soap.
-
Where Do Peanuts Come From
The peanut, while grown in tropical and subtropical regions throughout the world, is native to the Western Hemisphere. It probably originated in South America and spread throughout the New World